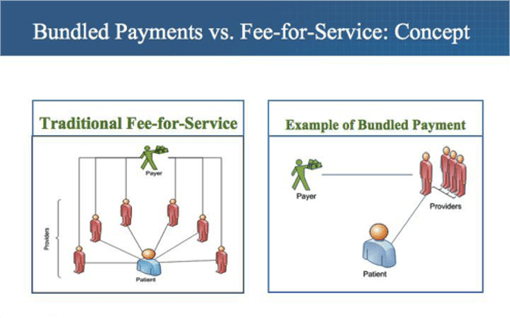
Rising healthcare costs account for 18% of our nation’s GDP. To put this into perspective for every $6 dollars the government spends $1 is on healthcare. Obviously these numbers are not sustainable and healthcare organizations have looked for alternatives to the standard fee for service model. The fee for service model rewards volume and does not focus on the quality of care provided. This means doctors can in essence be compensated for being inefficient. The answer to this issue lies in what are called bundled payments. Bundled payments solve this by promoting value over volume. This value as defined by the CMS is the set of health results that matter for the condition over the total cost of all necessary services over the care cycle. Bundled payments are a type of payment model that pays providers across the continuum of care a single sum of money for a tightly-defined set of clinical services over a set period of time. These forms of payments were more common in the early part of the 20th century but were phased out. However, CMS’ Medicare initiatives have tried to bring about the reemergence of bundle payment plans via models like the clinical episode payment model. Examples of these include BPCI Advanced, CJR, and the Oncology Care Model. The incorporation of bundle payment doesn’t stop there as now commercial and employer settings are also incorporating bundled payments. Bundled Payments are a single risk adjustment payment for the care of a condition.
It covers the full set of services and facilities needed to treat the condition over the full care cycle or a defined time period for chronic condition and primary care. It is contingent on condition-specific outcomes. However, there is a risk for the difference between the bundled price and the cost of all included services for the condition. This is known as limits of responsibility for unrelated care and outliers. Healthcare organizations using this payment method must be accountable for outcomes and cost condition by condition. Nonetheless, this model is definitely the best at achieving the main goal of healthcare, providing efficient and quality medical attention. This simply isn’t done in other plans like fee for service and capitation. Under capitation providers only receive a certain set amount of money that they can use to care for a patient. This is to help prevent the overuse of tests, imaging, drug administration, and etc. However, it does not solve the fundamental issue of focusing on curing the specific condition. This is where bundled payments differ as they deliver value patient by patient and condition by condition. Overall, they lead to an increase in patient satisfaction because bundled payment hold providers accountable for patient outcomes. Providers, patients, insurance companies, and employers all are responsible for the institution of the bundled payment system. Bundled payments drive multidisciplinary care, rewards good outcomes, incentivize improving efficiency, expand patient choices, creates competition & transparency by condition, and focus on areas of excellence. Most importantly, it generates competition on the most important feature of HC, which is value.