Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.

The 21st century has seen a major shift in how medicine has been provided and regulated historically. With that being said, the doctors of today are not equipped to take account of the importance of efficiency in their day to day practice. As medical spending continues to skyrocket throughout America it has become more and more imperative that physicians need to have the skill set to integrate both business skills of management/administration alongside practicing medicine with the main goal of decreasing exuberant medical costs. As a future physician, I have witnessed how unstainable the current practice of medicine is in certain regions of America and believe my coursework as a Masters in Healthcare Administration student will provide me with the toolset to help alleviate the escalating problem. Having graduated with a Bachelors in Biomedical Sciences from the University of Texas Rio Grande Valley I’ve gained knowledge in the “hard” sciences of anatomy, physiology, microbiology and many more subjects that will help me along this path of medicine. However, what I find impacted me the most throughout my time in the Rio Grande Valley was not what I learned in the classroom but what I was able to observe first hand. As a freshman interested in public health and epidemiology research, I was able to collect Type II Diabetic patient data and correlate them with answers from a survey that assessed Medical and Social Barriers these patients might face regularly. This study was conducted at a Federally Qualified Health Center known as the Brownsville Community Health Center. Many of the patients here are dependent on Medicare, Medicaid, Migrant Farm Worker insurance, and other federally sponsored health insurances. While there are millions being spent in the RGV barriers continue to exist which raises the question of whether doctors are being efficient. In fact, Medicare Spending here is $15,000 per enrollee which is twice the national average yet patient health seems to not be improving in the long term. I believe the solution to these issues lies in the integration of nanotechnology, digital health, and effective hospital management that will keep patient care at a high level while minimizing the unnecessary costs.

The medical field continues to evolve through the era of sterile techniques and antibiotics to the development of advanced imaging modalities into the last decades embrace of big data and informatics. Each advancement has taken time to be fully implemented in medical care, however, each iteration has improved patient outcomes over the last century. I believe the next evolution in medicine lies in the integration of artificial intelligence and machine learning with patient outcomes data. With more physicians seeing more patients and documenting encounters and results on electronic medical records, a plethora of data is being collected daily by hospitals and clinics around the country and even the world. It will be impossible for humans to sift through all these data points to draw conclusions, however, AI will provide an avenue through which patient care and outcomes can be studied in a comprehensive and specific manner to draw inferences with statistical power. I completed a research project at the Brownsville Community Health Center where I created a database to study risk factors and the management of patients with T2DM and their respective HbA1C levels. This experience brought to light actionable goals in patient care and highlighted the need for more robust data mining and the need for algorithms to automate the data collection and analysis. However, AI will not replace the need for caring physicians who can take the analyzed data and develop care plans tailored to their communities and to their individual patients.
In this week’s blog post I will recap what I learned from a Webinar titled “Better Outcomes and Lower Costs – It Starts at the Point of Care”. The panelists on the webinar were medical doctors, Dr. Tom Schweiterman and Dr. Mechley, and the moderator was Mr. Rubenfire who works as a Custom Content Strategist at Modern Healthcare. I found this webinar very informative as I’m going to be a Medical Student this upcoming year and I intend to use what I have learned as an MHA to improve clinical quality when I begin to practice. The major takeaways from this webinar were identifying cost management, learning how to improve workflow to better patient and provider satisfaction, and how providers can optimize the work of clinicians to ensure that they have accurate and actionable data at the point of care. Overall, I learned a lot from this webinar and cannot wait to utilize these skills in my medical practice.

The question of whether patient experience and financial performance is correlated has long been asked. The answer to this question is that like any consumer based industry patient experience is a huge determinant on the financial performance of healthcare organizations. For example, look at your own life what do you do when you feel sick? Most people go to a doctor! This is where customer service, quality of care, value, and etc. all come in to play as patients are the sole evaluators of their care. In the world we live in social media, yelp, google reviews, and etc. all play a role in how we perceive the quality of a business or medical practice. If patient X publicizes that Houston Methodists’ hospital staff were rude and unorganized this generates a negative image of the hospital system that could persuade patients to take their medical needs elsewhere. The market for healthcare is fierce and especially here in Houston we have access to world class doctors and hospitals making each and every opinion valuable. In a CMS data report analyzing nearly 1400 inpatient acute care hospitals, researchers found that patient experience did indeed have an impact on the financial performance on the hospitals. In these hospitals there was a positive relationship with cash flow margins and operating profit margins across for-profit, non-profit, and governmental hospitals. As I mentioned in another one of my blog posts, payment plans like bundled payments are the best way at keeping patient experiences positive while still sustaining strong financial success. When physicians are compensated based on how they treat patients case by case and condition by condition rather than as a generalized population patient outcomes are better. This patient-centered model is key and promotes the main thesis of medicine: providing empathetic care in a cost-effective manner.
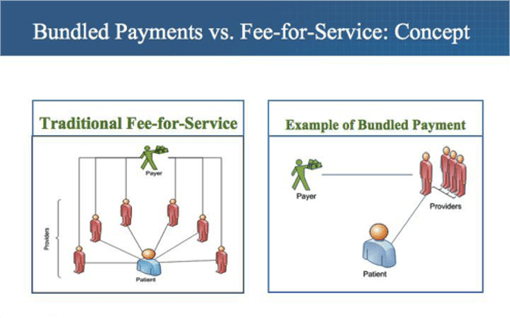
Rising healthcare costs account for 18% of our nation’s GDP. To put this into perspective for every $6 dollars the government spends $1 is on healthcare. Obviously these numbers are not sustainable and healthcare organizations have looked for alternatives to the standard fee for service model. The fee for service model rewards volume and does not focus on the quality of care provided. This means doctors can in essence be compensated for being inefficient. The answer to this issue lies in what are called bundled payments. Bundled payments solve this by promoting value over volume. This value as defined by the CMS is the set of health results that matter for the condition over the total cost of all necessary services over the care cycle. Bundled payments are a type of payment model that pays providers across the continuum of care a single sum of money for a tightly-defined set of clinical services over a set period of time. These forms of payments were more common in the early part of the 20th century but were phased out. However, CMS’ Medicare initiatives have tried to bring about the reemergence of bundle payment plans via models like the clinical episode payment model. Examples of these include BPCI Advanced, CJR, and the Oncology Care Model. The incorporation of bundle payment doesn’t stop there as now commercial and employer settings are also incorporating bundled payments. Bundled Payments are a single risk adjustment payment for the care of a condition.
It covers the full set of services and facilities needed to treat the condition over the full care cycle or a defined time period for chronic condition and primary care. It is contingent on condition-specific outcomes. However, there is a risk for the difference between the bundled price and the cost of all included services for the condition. This is known as limits of responsibility for unrelated care and outliers. Healthcare organizations using this payment method must be accountable for outcomes and cost condition by condition. Nonetheless, this model is definitely the best at achieving the main goal of healthcare, providing efficient and quality medical attention. This simply isn’t done in other plans like fee for service and capitation. Under capitation providers only receive a certain set amount of money that they can use to care for a patient. This is to help prevent the overuse of tests, imaging, drug administration, and etc. However, it does not solve the fundamental issue of focusing on curing the specific condition. This is where bundled payments differ as they deliver value patient by patient and condition by condition. Overall, they lead to an increase in patient satisfaction because bundled payment hold providers accountable for patient outcomes. Providers, patients, insurance companies, and employers all are responsible for the institution of the bundled payment system. Bundled payments drive multidisciplinary care, rewards good outcomes, incentivize improving efficiency, expand patient choices, creates competition & transparency by condition, and focus on areas of excellence. Most importantly, it generates competition on the most important feature of HC, which is value.
This is an example post, originally published as part of Blogging University. Enroll in one of our ten programs, and start your blog right.
You’re going to publish a post today. Don’t worry about how your blog looks. Don’t worry if you haven’t given it a name yet, or you’re feeling overwhelmed. Just click the “New Post” button, and tell us why you’re here.
Why do this?
The post can be short or long, a personal intro to your life or a bloggy mission statement, a manifesto for the future or a simple outline of your the types of things you hope to publish.
To help you get started, here are a few questions:
You’re not locked into any of this; one of the wonderful things about blogs is how they constantly evolve as we learn, grow, and interact with one another — but it’s good to know where and why you started, and articulating your goals may just give you a few other post ideas.
Can’t think how to get started? Just write the first thing that pops into your head. Anne Lamott, author of a book on writing we love, says that you need to give yourself permission to write a “crappy first draft”. Anne makes a great point — just start writing, and worry about editing it later.
When you’re ready to publish, give your post three to five tags that describe your blog’s focus — writing, photography, fiction, parenting, food, cars, movies, sports, whatever. These tags will help others who care about your topics find you in the Reader. Make sure one of the tags is “zerotohero,” so other new bloggers can find you, too.